Cardiac Catheterizations for Heart Defects
Therapeutic cardiac catheterizations for children
A therapeutic cardiac catheterization is a procedure to treat your child's heart defect. A doctor will use special techniques and a thin plastic spaghetti-like tube or catheter that goes to the heart from blood vessels in the leg or neck. These techniques allow the repair to be done without surgically opening the chest and heart. The types of defects that can be repaired include closing a hole in the wall that separates the heart’s right and left sides, widening a narrowed vessel or stiff valve, and closing abnormal blood vessels using a variety of devices.
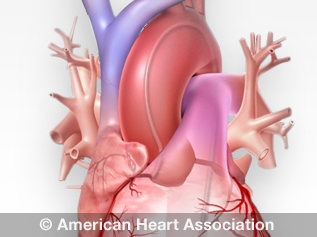
See an illustration of cardiac catheterization
Before the cardiac catheterization procedure
Before entering the cardiac catheterization laboratory (cath lab), an IV will be started and a medication may be given to help your child relax and fall asleep. Vital signs will be monitored before and during the procedure.
Your child may just be sedated or may have to undergo general anesthesia. If general anesthesia is needed, a breathing tube is inserted into the airway to make breathing easier. Additional medications and fluids may be given throughout the procedure to keep your child comfortable.
The cardiac catheterization procedure
After your child is asleep, the part of the body where the catheters will be inserted is prepared by washing the skin with an antiseptic solution to ensure that it’s clean. Additional sedation may be given as needed.
During the therapeutic cardiac catheterization, specialized tubes called sheaths are placed into the blood vessels in the groin or neck area. This allows the doctor to get catheters through these vessels and into the heart. In the newborn period, the “belly-button” vessels (the umbilical vessels) may be used for access to the heart. A local anesthetic is generally used before placing catheters and sheaths in the body.
The movement of these catheters as they pass from one heart chamber to the next is carefully monitored with X-ray images on a TV screen in the cath lab. Through the catheters, pressures are measured and blood samples are drawn from various sites within the heart. This gives the doctor valuable information about your child’s heart function and the blood flow through the heart and lungs. Contrast (X-ray dye) is injected through the catheters to get a clear moving picture of internal heart structures to identify where the defect is and how severe it is. This information helps your doctor determine the best way to treat the defect.
The catheter’s movement can cause abnormal heart rhythms. Your doctor can usually treat these rhythms by moving or removing the catheter. Rarely, the catheter can interfere with the heart’s electrical system. This is known as heart block. Although this is usually temporary, placing a special catheter connected to an electrical battery (pacemaker) may be required until the heart’s electrical system corrects itself.
When the procedure is complete, all catheters and sheaths are removed. This is similar to removing an IV. For several minutes pressure is put on the spot where the catheters were inserted. To prevent bleeding, a pressure dressing may be applied.
Your child is then transferred to the recovery area.
After catheterization
When your child arrives in the recovery area, he or she will be monitored closely. If your child was treated under general anesthesia, the breathing tube will be removed as soon as your child is breathing without assistance. Occasionally, a medicine to prevent nausea and vomiting may be given.
Discharge
Patients can be discharged that same day, but sometimes an overnight hospital stay is required. Your doctor will decide when your child can go home.
Before discharge, your doctor or nurse will give you follow-up instructions. These will describe how to take care of the dressing and the insertion site. Be sure to call your health care team if your child experiences any symptoms including bleeding that can’t be stopped, chest pain, fever, increased pain or swelling, or anything else you are concerned about.
If you have questions or concerns about your child’s health, contact your cardiologist.
Types of therapeutic cardiac catheterization
In the last two decades, tremendous medical advances have allowed congenital heart defects to be treated in the cath lab without surgery.
Valvuloplasty or balloon valvotomy
This procedure is done to open a narrowed heart valve. It is most commonly used to open the valves connecting the heart to the lungs (pulmonary valve) or to the body (aortic valve). The problem may occur because the valve is too narrow or the flaps formed incorrectly at birth. This makes it harder for the heart to pump blood to the lungs or to the body. It’s like asking someone to breathe through a straw. The narrower the straw, the harder it is to breathe.
To open the narrowed valve, a special catheter with a balloon attached to its end is used. This catheter is advanced from a blood vessel in the groin or neck through the narrowed valve. Then the balloon is inflated to widen the opening.
Angioplasty
This procedure widens a narrowed blood vessel. These narrowings are often associated with congenital heart defects and can occur naturally or after surgery. Similar to a narrowed valve, a narrowed vessel restricts blood flow and causes the heart to work harder.
The procedure used is similar to a valvuloplasty in that a balloon catheter is placed inside the narrowed blood vessel and expanded to stretch open the vessel.
Stent implantation
Sometimes, simply widening a narrowed blood vessel with a balloon isn’t effective. In this situation, a stent is used to provide structural support within the narrowed vessel to keep it wide open. Stents are metal mesh tubes. They’re designed to stretch open inside a narrowed blood vessel and hold the vessel wall open.
The most common types of stents used in children are “balloon-expandable” stents. These are mounted onto a balloon and positioned at the site of narrowing through a long sheath. Then the balloon is inflated to expand the stent against the narrowed vessel wall. The stent is opened to the appropriate size depending on the patient’s size. The balloon is deflated and removed while the stent stays in the vessel to keep it from narrowing.
After stent implantation, your child will usually be placed on a blood-thinning medicine, such as aspirin, to help keep clots from forming.
Implanted stents don’t activate metal detectors. Magnets and microwaves don’t affect the stent or the surrounding heart tissue and blood vessels.
Balloon and blade septostomy
In some special circumstances, it’s necessary to create a larger hole between the walls of the heart’s upper chambers (the right and left atrium). Special balloons and blade catheters are used to create these openings to increase blood flow between the heart’s upper chambers.
Valve perforation
Some patients are born with a completely blocked pulmonary valve. This is the valve that controls blood flow from the right ventricle (lower chamber of the heart) to the main pulmonary artery, which carries blood from the heart to the lungs. This is called pulmonary atresia. The treatment will depend on the blockage’s severity.
- In some cases, blood flow can be improved with cardiac catheterization. During this procedure, doctors can expand the valve using a balloon or they may need to place a stent (a small tube) to prop open the ductus arteriosus, a blood vessel in the fetal circulation that connects the pulmonary artery to the aorta. (The ductus arteriosus typically closes within days or weeks after birth.)
- In most cases of pulmonary atresia, a baby may need surgery soon after birth to open or replace the valve.
Most babies will need regular follow-up care from a health care professional as they get older.