Choosing the Right Stroke Rehab Facility
Rehabilitation should begin as soon as the patient stabilizes. Generally, this first stage of rehabilitation occurs in the hospital. In planning for discharge from the hospital, the patient and their family, with the support of the social workers or case manager, must determine the best place for care. Many patients return home, but others benefit from time in a rehabilitation program to continue recovery.
Keep in mind that the services available in the different types of facilities is broad and the intensity of rehabilitation care varies widely depending on the setting. Here is a closer look at the different types and facilities and how they differ:
Inpatient Rehabilitation Facilities (IRFs)
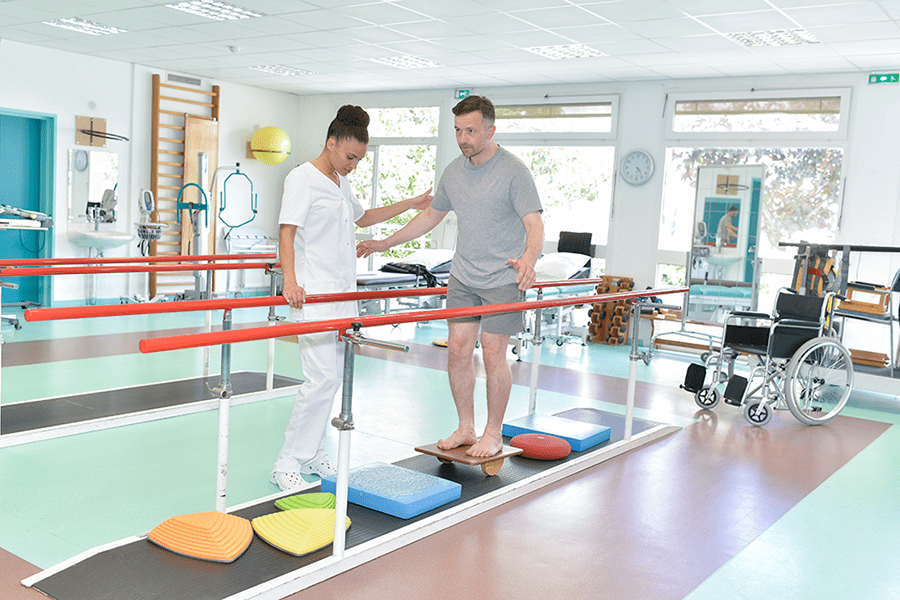
Inpatient rehabilitation may be located independently or may be part of a large hospital complex. These facilities provide hospital-level care to stroke survivors who need intense 24-hour a day care under the direct supervision of a rehabilitation physician. Patients usually remain in the facility for two or three weeks and participate in an intensive, coordinated rehabilitation program. These programs often include at least three hours per day of physical, occupational and speech therapy for at least five days a week.
Skilled Nursing Facilities (SNFs)
The rehabilitation services available in SNFs are for patients who no longer need hospital care but still require some nursing services and a less intensive rehabilitation program with fewer hours of required therapy participation. Your care must follow a physician’s plan, but a physician does not provide daily direct supervision.
Long-Term Acute Care Hospitals
Long-term acute care hospitals provide extended medical and rehabilitation care to people with complex medical needs, such as patients who require regular ventilation. These hospitals provide care to a relatively small number of stroke patients.
Nursing Homes
These long-term residential care facilities are for those who are unable to live in their community. Patients no longer need full hospital care but still require 24-hour access to nursing support. Rehabilitation services may be offered to people in these facilities as they qualify.
Home and Out-Patient Rehabilitation Programs
Services may include skilled nursing care, rehabilitation to limited assistance with daily tasks.
From home, patients may travel to a rehabilitation facility or clinic, which may stand alone or be connected to a hospital complex. Participating in a facility offers access to a wide range of treatments and therapists. Rehabilitation can also be provided in the home. These arrangements are usually the most convenient for people who don’t have transportation or who require treatment from a single type of rehabilitation therapist.
Patients who depend on the Medicare program for rehabilitation must meet Medicare’s requirements and be certified as “homebound” by their health care professional to qualify for these services. Currently, lack of transportation is not a valid reason to receive home therapy. The biggest disadvantage of home rehabilitation is the lack of specialized equipment. However, performing treatment at home gives people the advantage of practicing skills and developing compensation strategies within their own environment.
Tele-Rehabilitation
Tele-rehabilitation has emerged as a viable option for continued rehabilitation support once the stroke survivor returns home or when transportation or distance to continue receiving services come into play. Tele-rehab can include:
- Education
- Information
- Remote monitoring with feedback and care plans
- Demonstration and practice of daily activities
- Other types of support
Rehabilitation can build your strength, capability and confidence. It can help you continue your daily activities despite the effects of your stroke. It’s an essential part of stroke care!
Home and Out-Patient Rehabilitation Programs in Spanish
Accredited Rehabilitation Facilities
The Commission on the Accreditation of Rehabilitation Facilities (Carf) is an international nonprofit accrediting body. Carf provides accreditation in the human services field — focusing on the areas of rehabilitation, employment and community, child and family, and aging services.
Visit Carf for a list of accredited rehabilitation facilities and other valuable information.
You and your family need to be involved when choosing a facility. Start with these questions:
What types of rehab care will my insurance cover?
Do you have a stroke rehab program, and if so, how many patients are in it?
How do you assure high-quality care? How do you evaluate progress?
What percentage of your short-term residents are successfully discharged home?
Where does rehab occur? What therapy programs are available?
How do you prepare me to return home?
How do you help caregivers?
What is done to help prevent falls?
Questions to ask your doctor before your loved one is discharged:
What is the extent of my/my loved one’s stroke damage? What areas of the brain have been affected?
What is the prognosis and expected course for recovery?
What types of services are likely to improve the outcome?
Does this depend on the areas of the brain where the stroke caused damage?
What is my/my loved one’s ability to participate and engage in various post-acute services?
What is my/my loved one’s underlying medical/health situation and complexity, and what other medical services will be required?
Questions to ask about or directly to the post-acute setting(s):
Is the rehab facility certified to care for people with a stroke?
What is the maximum amount of rehabilitation services I/my loved one can receive?
How intense will it be?
What medical services are available?
What special clinical training do the nurses, social workers and dietitian have?
How does the setting measure functional recovery, and what outcomes are typical for stroke patients?




